GASTROESOPHAGEAL REFLUX.?
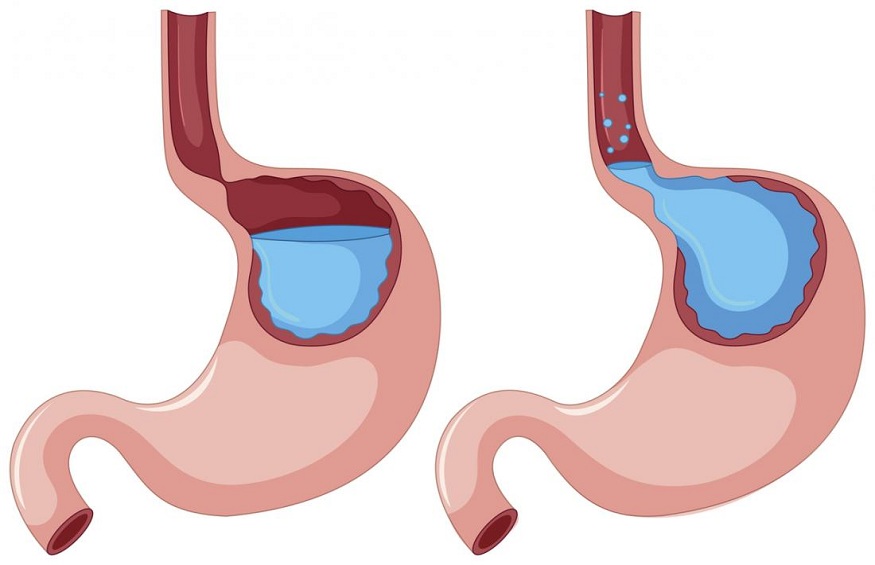
Gastroesophageal reflux disease (GERD) is defined as the set of bothersome symptoms or complications related to the passage of gastric contents into the esophagus. There is a physiological GERD (in everyone) especially after meals,
EPIDEMIOLOGY
GERD is a frequent pathology, most often benign, but which can significantly alter the quality of life of patients. It is considered in France that 30% of adults have occasional symptoms of GERD (at least once a month), and 5 to 10% frequent symptoms (weekly). Mucosal lesions are rarer: 20 to 30% of patients have ulcerated esophagitis, 5 to 10% have complications such as Barrett’s esophagus (precancerous state) or peptic stenosis (narrowing of the esophagus).
GERD DIAGNOSIS
The diagnosis of GERD is most often clinical, especially in the presence of typical signs such as heartburn, acid regurgitation and postural syndrome. It is in the event of atypical symptoms that additional examinations can be useful. We can find epigastric burns, retro-sternal chest pain, chronic cough, difficult to control asthma, ENT symptoms such as hoarseness, chronic laryngitis. However, the imputability of GERD in these pulmonary or ENT symptoms remains controversial and has been greatly overestimated, especially in the absence of typical symptoms.
Faced with typical signs and in the absence of warning signs, the diagnosis of GERD is clinical and does not require any additional examination.
The esophagogastroduodenal fibroscopy (FOGD) allows to search for a differential diagnosis or complications. The indications for FOGD are as follows: isolated atypical symptoms; warning signs (weight loss, anemia, dysphagia, gastrointestinal bleeding); age > 50 years; resistance to initial treatment or early relapse on discontinuation of treatment. In the presence of esophagitis, EBO or peptic stenosis, the positive diagnosis of GERD is affirmed.
pH-metry establishes the positive diagnosis of GERD by detecting and quantifying episodes of reflux. It is indicated if the symptoms are atypical and the FOGD normal, or if the symptoms are resistant to well-conducted treatment. The pH-impedancemetry indicates, in addition to the pH, the liquid or gaseous nature of the contents of the esophagus, adding the detection of non-acid or slightly acid reflux to that of acid reflux.
H2 blockers (cimetidine, ranitidine, etc.) are less effective than PPIs in both symptom relief and esophageal healing. In addition, their use is limited by a gradual exhaustion of their effect, which does not allow them to be used over the long term to prevent recurrence. They currently mainly retain a place in children or as an alternative to PPIs.
GERD surgery aims to strengthen the anti-reflux barrier by fundoplication, a technique consisting of folding a portion of the proximal stomach around the lower esophagus so as to form a valve, circumferential (Nissen intervention) or partial (Toupet intervention) , preferably laparoscopically. It is very effective in controlling the symptoms of GERD (85% success at 5 years in expert centres). It exposes to more or less severe side effects, such as persistent dysphagia, inability to vomit or belch, flatulence, dyspeptic disorders.
Therapeutic strategy
The therapeutic objectives are the relief of symptoms, the healing of the mucosa in case of esophagitis and the prevention of recurrence. In the majority of cases, the diagnosis of GERD is easy; treatment can be prescribed immediately without further investigation. If the symptoms are occasional (< once a week) and not very disabling, topical treatment on demand may be sufficient. If the symptoms are frequent (> 1 time per week), typical without alarm signs, it is recommended to introduce treatment with PPI at half a dose. If symptoms are more frequent and/or severe, PPIs can be given in a single dose. If effective, PPIs are continued for four weeks. In the long term, PPI treatment can be maintained, by finding the minimum effective dose continuously or on demand,
In case of warning signs or in a patient over 50 years old, endoscopy is essential before treatment to detect a complication. When the symptoms are atypical, a test treatment can be attempted as first intention but additional explorations (endoscopy, pHmetry) will be necessary in any case to document a possible reflux in the event of ineffectiveness or if a long-term treatment is envisaged. .
The indications for surgery must be well thought out because of the possible side effects. Paradoxically, the best candidates for surgery are patients whose symptoms are perfectly relieved by PPIs but who do not tolerate them or do not want long-term treatment. Conversely, the ineffectiveness of PPIs is a factor in the failure of surgery. In fact, more than half the time, the symptoms not relieved by PPIs cannot be attributed to reflux, acid or not. In this case, the diagnosis must be called into question and additional investigations carried out to document GERD.
CHALLENGES AND PROSPECTS
One of the issues in the management of GERD is the long-term prescription of PPIs. In addition to the problem of the cost of these treatments, which are among the most prescribed, several risks possibly linked to the chronic use of PPIs have been raised: osteoporosis and increased risk of fracture (neck of the femur, vertebral compression), cardiovascular problems , kidney failure, vitamin deficiencies, gastrointestinal and pulmonary infections. The published data are contradictory, with the exception of intestinal infections, the risk of which is proven but low. When it is necessary, the benefit of a PPI treatment is very much greater than the possible, unproven risks that it could entail. Caution should be exercised when using PPIs in frail, elderly or hospitalized people.
The other major challenge is screening for precancerous lesions of the oesophagus. The incidence of lower esophageal adenocarcinoma is increasing due to the high prevalence of obesity, a risk factor for both cancer and GERD, favoring the occurrence of Barrett’s esophagus. It is therefore necessary to promote the use of screening endoscopy for Barrett’s esophagus in patients at risk with symptoms of GERD (age over 50 years, obesity, symptoms requiring long-term treatment).